How much is 2 herniated disc settlements
The quantity of an agreement for a herniated disc injury can range widely relying on numerous elements, inclusive of the severity of the damage, the impact for your life and capacity to paintings, clinical charges, misplaced wages, ache and suffering, and the jurisdiction where the case is being settled. It’s essential to discuss with a private harm attorney who can compare your specific state of affairs and offer guidance on what might be a reasonable agreement amount. They can recall all these elements and negotiate to your behalf to try and steady the satisfactory viable final results.
How long to recover from herniated disc
The restoration time for a herniated disc varies substantially relying on elements which include the severity of the herniation, the man or woman’s normal health, the treatment acquired, and adherence to rehabilitation physical games. In many cases, symptoms of a herniated disc can enhance within some weeks to 3 months with conservative remedies which includes rest, physical remedy, pain management, and possibly steroid injections.
For a few humans, in particular those with greater excessive herniations or underlying health troubles, healing might also take longer, potentially several months or even up to a yr. In cases wherein conservative treatments do no longer offer enough alleviation, surgical operation can be taken into consideration, which can also affect recovery time.
It’s critical to work intently with healthcare specialists to expand a remedy plan tailor-made in your unique condition and desires. They can reveal your development and make modifications on your treatment as essential to optimize healing and limit the risk of long-term headaches.
Can a herniated disc cause permanent nerve damage?
Yes, a herniated disc can potentially reason permanent nerve damage, especially if it leads to extended compression or inflammation of the nerves. When the gel-like cloth from in the disc pushes out and presses towards nearby nerves, it can cause infection, ache, numbness, tingling, and weak spot within the affected location.
If the compression or irritation persists for an extended period, it could bring about damage to the nerves, which might also end up permanent. This can lead to persistent ache and other signs and symptoms even after the herniated disc itself has healed or been treated.
Prompt and suitable medical care, which include interventions to relieve pressure at the nerves and manage signs, can assist limit the danger of everlasting nerve damage. This might also consist of remedies consisting of physical remedy, medicine, injections, and in a few instances, surgery to take away the herniated portion of the disc. Early diagnosis and intervention are key to preventing or minimizing long-term complications.
What does a herniated disc look like on an mri
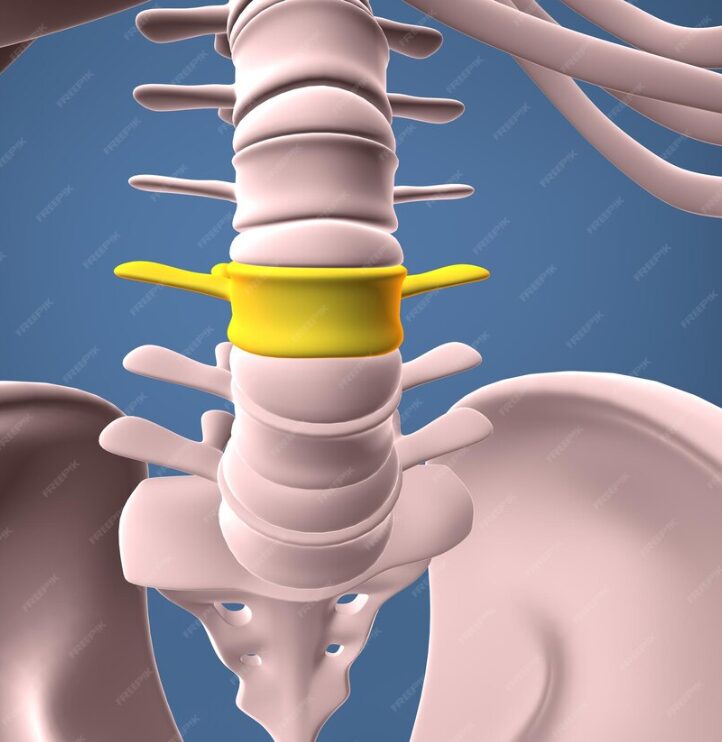
On an MRI (Magnetic Resonance Imaging), a herniated disc generally seems as a protrusion or bulge of the disc fabric beyond the normal obstacles of the disc area. Here are some characteristics of a herniated disc that may be visible on an MRI:
Protrusion/Bulge: The disc fabric might also protrude outward from its normal position, extending into the spinal canal or the space where nerves exit the spinal twine.
Disc Material Leakage: The gel-like material within the disc, known as the nucleus pulposus, may additionally leak out through a tear or rupture in the hard outer layer of the disc, known as the annulus fibrosus. This can bring about a seen displacement of disc cloth.
Compression of Nerve Roots: In some instances, a herniated disc may additionally compress or aggravate close by nerve roots as they exit the spinal twine. This compression can be seen as a narrowing of the gap around the nerve roots or direct contact among the herniated disc cloth and the nerves.
Inflammation: Surrounding tissues can also display signs of infection in response to the herniation, which also can be visible on an MRI.
Overall, the MRI affords unique pictures that allow healthcare vendors to assess the extent and area of the herniated disc, in addition to any associated nerve compression or harm. This records allows manual remedy choices and prognosis for the individual experiencing signs related to the herniated disc
Can a herniated disc cause headaches?

While headaches are not generally at once caused by a herniated disc in the spine, there are some oblique approaches wherein a herniated disc ought to potentially make a contribution to complications:
Muscle Tension and Posture: Pain and discomfort from a herniated disc, specifically in the cervical (neck) vicinity, can cause muscle tension and adjustments in posture. These factors can make contributions to tension-type complications or cervicogenic headaches, which originate from the neck.
Nerve Irritation: If a herniated disc inside the cervical backbone is severe enough to compress or worsen nerves in the neck, it is able to motive ache that radiates into the pinnacle, doubtlessly main to headaches. This type of pain is often described as radiating or taking pictures from the neck into the head.
Altered Spinal Mechanics: A herniated disc can have an effect on the biomechanics of the spine, leading to compensatory movements and adjustments in spinal alignment. These modifications may additionally contribute to muscle imbalances, tension, and strain, which could indirectly make contributions to complications.
It’s important to be aware that complications could have numerous reasons, and a thorough assessment by using a healthcare expert is important to determine the underlying reason for the complications. If you’re experiencing chronic complications together with signs of a herniated disc, it is important to talk about your signs with a physician for correct diagnosis and control.
How long to wait to run after herniated disc
The amount of time you must wait earlier than resuming going for walks after a herniated disc can vary depending on several elements, together with the severity of your injury, the remedy you received, and the way your frame responds to healing. Here are a few preferred tips:
Follow Medical Advice: First and major, it is vital to observe the recommendation and suggestions of your healthcare issues, such as a doctor or physical therapist. They can determine your precise situation, reveal your progress, and offer steering on while it’s safe to resume jogging.
Gradual Return to Activity: If your healthcare issuer clears you to renew running, it’s crucial to do so regularly and carefully. Start with shorter distances and lower intensity, and step by step growth the period and depth of your runs through the years. This slow approach permits your body to adapt to the demands of going for walks while minimizing the risk of re-damage.
Listen to Your Body: Pay close attention to how your frame responds to jogging. If you experience increased ache, discomfort, or different symptoms at some point of or after running, it can be a signal which you need to reduce or alter your activity degree. Pushing via ache should get worse your circumstance and put off your restoration.
Focus on Proper Form and Technique: Pay interest in your walking shape and method to decrease strain to your spine and reduce the threat of re-damage. Maintaining desirable posture, attractive your middle muscle mass, and averting immoderate twisting or jarring moves can help shield your spine while strolling.
Consider Low-Impact Alternatives: If strolling exacerbates your signs and symptoms or in case your healthcare provider recommends against it, remember low-impact alternatives which include on foot, swimming, cycling, or the usage of elliptical machines. These activities can offer cardiovascular advantages with much less strain to your backbone.
Ultimately, the decision to renew strolling after a herniated disc need to be made in session together with your healthcare company, taking into account your man or woman occasions and any guidelines or regulations they provide. Prioritize your health and protection, and be affected person with the recovery system to keep away from setbacks.
Is disc osteophyte complex the same as herniated disc?
No, disc osteophyte complex (also referred to as disc osteophyte complicated or degenerative disc disease with osteophyte formation) isn’t the same as a herniated disc.
Disc Osteophyte Complex: This time period refers to a condition where there is both degeneration of the intervertebral disc (the cushioning structure between the vertebrae inside the backbone) and the formation of osteophytes, which can be bony growths that expand along the edges of the vertebral our bodies. Disc osteophyte complex can result from put on and tear at the backbone through the years, leading to adjustments such as lack of disc peak, disc bulging, and the formation of bone spurs or osteophytes.
Herniated Disc: A herniated disc, additionally known as a slipped disc or ruptured disc, occurs whilst the internal cloth of the disc (nucleus pulposus) protrudes thru a tear or rupture inside the outer layer (annulus fibrosus) and extends beyond the disc’s ordinary limitations. This can result in compression or inflammation of nearby nerves, inflicting signs including pain, numbness, or weakness within the affected place.
While each disc osteophyte complicated and herniated discs are situations which could affect the intervertebral discs inside the backbone, they involve distinct mechanisms and feature awesome characteristics. Disc osteophyte complex is generally characterized by means of degenerative changes and bone spur formation, while a herniated disc involves the protrusion of disc cloth thru a tear or rupture inside the outer layer of the disc, potentially main to compression of nearby nerves.