What is Non-Obstructive Coronary Artery Disease (CAD)?
Nonobstructive coronary artery disease (CAD) is atherosclerotic plaque that would not be expected to obstruct blood flow or result in anginal symptoms.
Nonobstructive coronary artery disease refers to a condition in which there is atherosclerosis or plaque buildup in the coronary arteries, but the degree of narrowing or obstruction is not significant enough to cause flow-limiting blockages. In other words, while there may be some buildup of fatty deposits or plaques in the coronary arteries, these deposits do not severely restrict blood flow to the heart muscle.
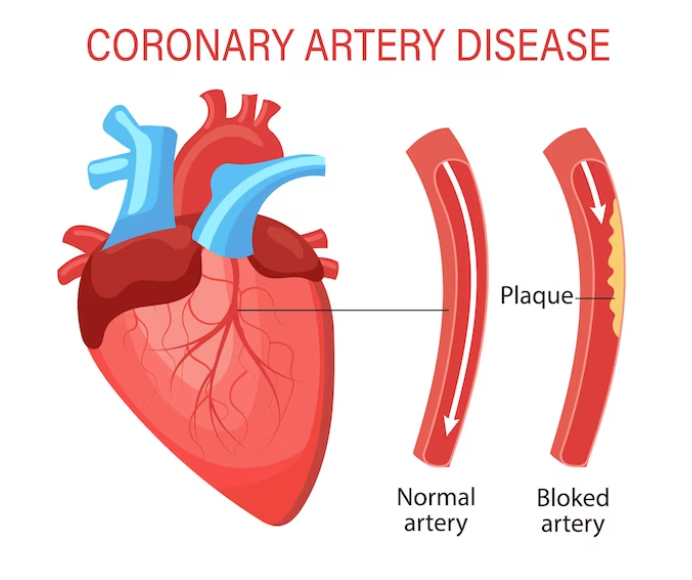
Coronary artery disease (CAD) is a condition characterized by the accumulation of plaque, which is made up of cholesterol, fat, calcium, and other substances, on the walls of the coronary arteries—the blood vessels that supply oxygen and nutrients to the heart muscle. Over time, these plaques can become larger and, in some cases, lead to the formation of blood clots or more severe blockages.
Nonobstructive CAD may be diagnosed through various imaging tests, such as coronary angiography, coronary computed tomography angiography (CCTA), or invasive coronary angiography. These tests allow healthcare providers to visualize the coronary arteries and assess the degree of narrowing.
It’s important to note that even nonobstructive CAD can have clinical significance. Plaques in the arteries may contribute to inflammation, affect blood vessel function, and, in some cases, lead to chest pain or other symptoms. Additionally, individuals with nonobstructive CAD may still be at risk for cardiovascular events, and management strategies, including lifestyle modifications and medications, may be recommended to reduce this risk.
Treatment and management of nonobstructive CAD often involve addressing risk factors, such as high blood pressure, high cholesterol, diabetes, and promoting heart-healthy habits like regular exercise, a balanced diet, and smoking cessation. Individualized care plans will be determined based on a person’s overall health, symptoms, and risk factors.
Obstructive CAD
Atherosclerosis is a condition characterized by the buildup of plaque on the walls of arteries. This plaque is composed of cholesterol, fats, calcium, white blood cells, and other substances. Over time, the accumulation of plaque can lead to the narrowing and hardening of the arteries, a process known as atherosclerosis.
When atherosclerosis occurs in the coronary arteries—the blood vessels that supply oxygen and nutrients to the heart muscle—it can lead to coronary artery disease (CAD). In CAD, the narrowed or blocked arteries can restrict blood flow to the heart, potentially causing chest pain (angina) or leading to more severe events such as heart attacks.
The term “obstructive CAD” is used when the narrowing of the coronary arteries is significant enough to limit or obstruct blood flow to the heart muscle. This obstruction is often caused by the presence of atherosclerotic plaques that reduce the diameter of the arteries.
Non-obstructive CAD
Non-obstructive CAD, while seemingly less severe, is also a major risk factor for heart attack.
Non-obstructive CAD can also cause angina, along with the following symptoms, which people with obstructive CAD often exhibit:
fatigue
heart palpitations
lightheadedness
pain in the arms, back, jaw, or neck
Non-obstructive CAD is not the result of atherosclerosis but refers to other types of coronary artery dysfunction, including:
damage to the endothelium (inner lining) of one or more coronary arteries
abnormal constriction of the coronary arteries (coronary vasospasm)
problems with the smaller blood vessels that branch off the main coronary arteries (microvascular dysfunction)
pressure from nearby heart muscle tissue (myocardial bridging)
What are the causes of non-obstructive coronary artery disease?
Non-obstructive coronary artery disease (CAD) can have various causes, and it’s often a multifactorial condition influenced by a combination of risk factors. Unlike obstructive CAD, where there is significant narrowing or blockage of the coronary arteries, non-obstructive CAD involves plaque buildup that does not severely impede blood flow. Some of the common causes and contributing factors to non-obstructive CAD include:
Early Stage Atherosclerosis: Non-obstructive CAD may represent the early stages of atherosclerosis, where there is some plaque formation on the arterial walls, but the degree of narrowing is not yet critical. This stage may not cause significant symptoms or flow limitations.
Microvascular Dysfunction: In some cases, non-obstructive CAD may be associated with dysfunction in the small blood vessels (microvasculature) of the heart. This can affect the ability of the coronary arteries to dilate and provide adequate blood flow to the heart muscle, even in the absence of significant plaque buildup.
Endothelial Dysfunction: Dysfunction of the endothelium, the inner lining of blood vessels, can contribute to non-obstructive CAD. Healthy endothelial function is crucial for maintaining blood vessel tone and regulating blood flow.
Inflammation: Chronic inflammation is a key factor in the development and progression of atherosclerosis. Inflammation can contribute to the formation of plaque in the coronary arteries, and non-obstructive CAD may be associated with inflammatory processes.
Risk Factors: Risk factors for atherosclerosis and CAD, such as high blood pressure, high cholesterol levels, smoking, diabetes, obesity, and a sedentary lifestyle, can contribute to the development of non-obstructive CAD.
Hormonal Factors: Hormonal changes, particularly in postmenopausal women, may influence the development of non-obstructive CAD.
Genetic Factors: A family history of cardiovascular disease can increase the risk of non-obstructive CAD. Genetic factors may play a role in how the body handles lipids (cholesterol and triglycerides) and responds to inflammation.
Autoimmune Conditions: Certain autoimmune conditions, such as rheumatoid arthritis or systemic lupus erythematosus, may be associated with an increased risk of cardiovascular disease, including non-obstructive CAD.
How is non-obstructive coronary artery disease diagnosed?
Non-obstructive coronary artery disease (CAD) is typically diagnosed through a combination of clinical evaluation, imaging tests, and other diagnostic procedures. Since non-obstructive CAD involves plaque buildup in the coronary arteries without significant narrowing or obstruction, specific imaging techniques are often used to visualize the arteries and assess their condition. Here are some common diagnostic methods:
Coronary Angiography:
Invasive Coronary Angiography: This procedure involves injecting a contrast dye into the coronary arteries, followed by X-ray imaging to visualize the blood flow and any abnormalities in the arteries. While traditional coronary angiography is excellent for detecting significant blockages, it may not provide detailed information about non-obstructive CAD.
Coronary Computed Tomography Angiography (CCTA):
CCTA Imaging: This non-invasive imaging technique uses computed tomography (CT) to obtain detailed images of the coronary arteries. It can provide information about the presence and extent of plaque in the arteries, even when there is no significant obstruction.
Intravascular Ultrasound (IVUS):
IVUS Imaging: In this procedure, a tiny ultrasound probe is inserted into the coronary arteries using a catheter. This allows for detailed imaging of the arterial walls and the detection of plaque buildup, including non-obstructive lesions.
Fractional Flow Reserve (FFR):
FFR Measurement: FFR is a test performed during coronary angiography or CCTA to assess the functional significance of a narrowing. While it is often used for obstructive lesions, it can also provide information about the hemodynamic significance of non-obstructive CAD.
Cardiac Magnetic Resonance Imaging (MRI):
MRI Imaging: Cardiac MRI can provide detailed images of the heart, including the coronary arteries. It may be used to assess blood flow and detect abnormalities, including non-obstructive CAD
How is non-obstructive coronary artery disease treated?
Treatment is determined by the nature of your non-obstructive coronary artery disease. Typically, managing the condition is done through lifestyle and clinical approaches.
Lifestyle changes
Mild cases of non-obstructive CAD that present no symptoms may not need treatment other than maintaining a healthy lifestyle.
If you’re experiencing angina or other symptoms, and your doctor determines that you may have endothelial or microvascular dysfunction, you may need to adopt more specific heart-healthy behaviors, including:
exercising for 30 to 40 minutes most days of the week
following a balanced diet, such as the Mediterranean or DASH diets
getting sufficient sleep
limiting alcohol intake
managing stress
no smoking
What is Coronary Artery Disease and Coronary Heart Disease?
Coronary artery disease (CAD) and coronary heart disease (CHD) are terms often used interchangeably, but they refer to slightly different aspects of a cardiovascular condition involving the heart and its blood vessels.
Coronary Artery Disease (CAD):
Definition: CAD is a broad term that encompasses the pathological processes occurring in the coronary arteries, which are the blood vessels that supply oxygen and nutrients to the heart muscle.
Characteristics: In CAD, there is atherosclerosis—a condition where fatty deposits, cholesterol, and other substances accumulate on the inner walls of the coronary arteries. This buildup, known as plaque, can lead to the narrowing or blockage of these arteries, reducing blood flow to the heart muscle.
Clinical Consequences: If left untreated, CAD can result in various clinical outcomes, including angina (chest pain or discomfort), myocardial infarction (heart attack), and other complications.
Coronary Heart Disease (CHD):
Definition: CHD specifically refers to the consequences of CAD on the heart muscle. It is a subset of CAD that focuses on the impact on the heart itself.
Characteristics: CHD can manifest as impaired blood flow to the heart muscle, leading to symptoms such as chest pain (angina) or shortness of breath. Severe blockages in the coronary arteries can result in heart attacks when blood flow to a part of the heart muscle is completely blocked, causing damage or death of that tissue.
Clinical Consequences: The clinical consequences of CHD can include angina, heart attacks, heart failure, and other complications related to the impaired function of the heart.
In summary, CAD is a broader term that encompasses the pathological changes occurring in the coronary arteries, while CHD specifically focuses on the impact of these changes on the heart itself. Atherosclerosis, the buildup of plaque in the coronary arteries, is a common underlying process in both CAD and CHD
How long can you live with Coronary Artery Disease?
The life expectancy for individuals with coronary artery disease (CAD) can vary widely and depends on several factors, including the severity of the disease, the effectiveness of treatment and management, overall health, lifestyle factors, and the presence of other medical conditions.
CAD is a chronic and progressive condition characterized by the buildup of plaque in the coronary arteries, which can lead to reduced blood flow to the heart muscle. The consequences of CAD can range from stable angina (chest pain or discomfort during physical activity or stress) to more severe conditions such as acute coronary syndrome (unstable angina or heart attack) and heart failure.
Key factors influencing life expectancy in individuals with CAD include:
Severity of CAD: The extent of blockages or narrowing in the coronary arteries plays a significant role. Severe and widespread blockages are associated with a higher risk of adverse events.
Effectiveness of Treatment: Early detection and appropriate management, including lifestyle changes, medications, and, in some cases, medical procedures (such as angioplasty or coronary artery bypass grafting), can contribute to better outcomes.
Comorbidities: The presence of other health conditions, such as diabetes, high blood pressure, and kidney disease, can affect life expectancy.
Lifestyle Factors: Healthy lifestyle choices, including a balanced diet, regular exercise, not smoking, and maintaining a healthy weight, can positively influence outcomes for individuals with CAD.
Medical Adherence: Adherence to prescribed medications and medical advice is crucial for managing CAD and preventing complications.
Access to Healthcare: Timely access to healthcare, including regular check-ups and follow-up appointments, is important for ongoing management.
It’s important to note that CAD is a manageable condition, and many individuals with CAD live long and fulfilling lives with appropriate treatment and lifestyle modifications. Advances in medical therapies and interventions have significantly improved outcomes for individuals with CAD. However, the condition requires ongoing attention and management.






Please tell me more about this. May I ask you a question?
Your articles are very helpful to me. May I request more information?
Sustain the excellent work and producing in the group!
The articles you write help me a lot and I like the topic
Thank you help me to promote it
You helped me a lot by posting this article and I love what I’m learning.
I’m so in love with this. You did a great job!!
Great content! Super high-quality! Keep it up!
Help me to promote my site
will be thankfull to you
Please provide me with more details on the topic
i am on it
Thank you for your help and this post. It’s been great.
You’ve been great to me. Thank you!
Thanks for posting. I really enjoyed reading it, especially because it addressed my problem. It helped me a lot and I hope it will help others too.
How can I find out more about it?
i am still writing on it will post it soon
When do we get more?
Here is the article
Here is the article
Please tell me more about your excellent articles
Your article helped me a lot, is there any more related content? Thanks!
Your article helped me a lot, is there any more related content? Thanks!