What is colonoscopy?
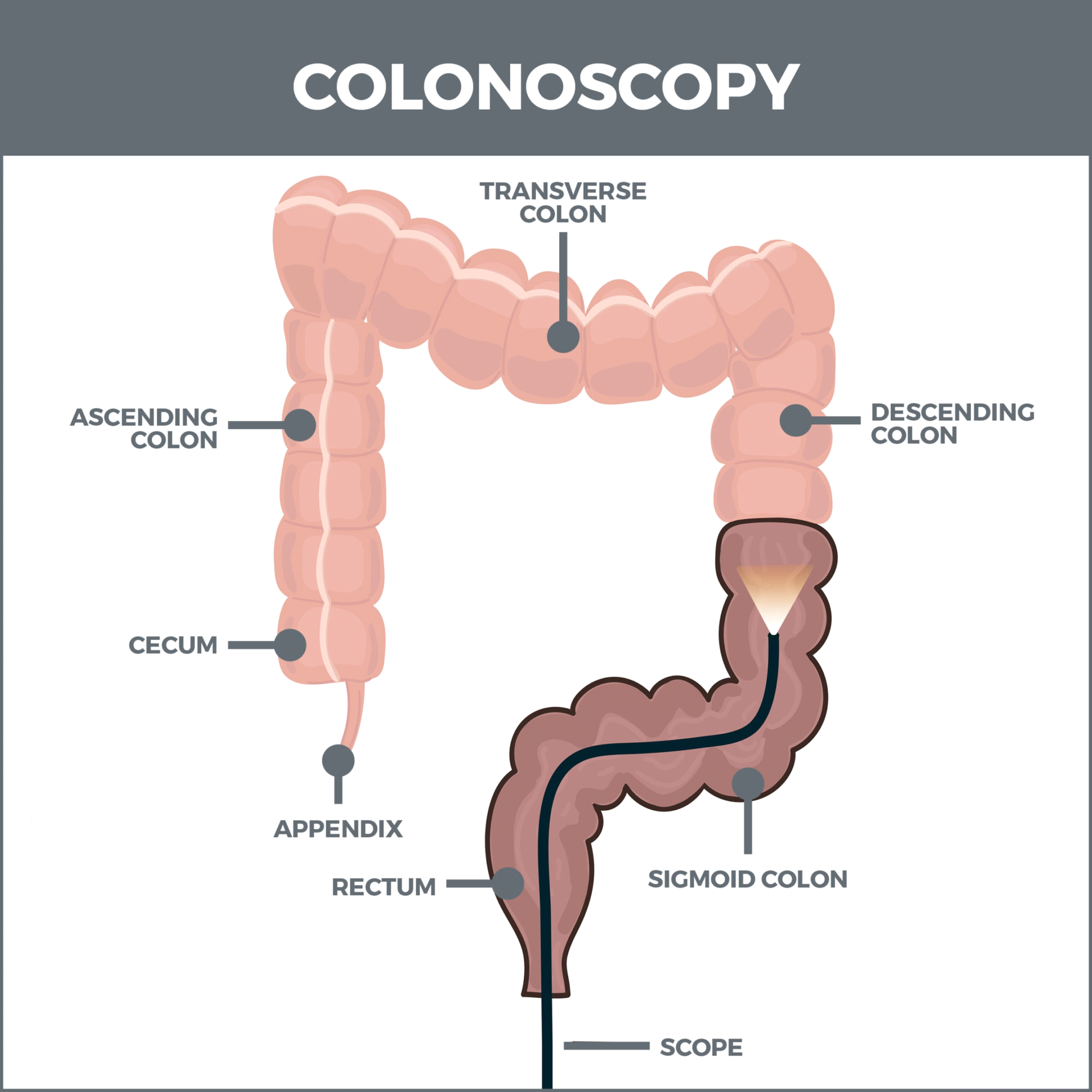
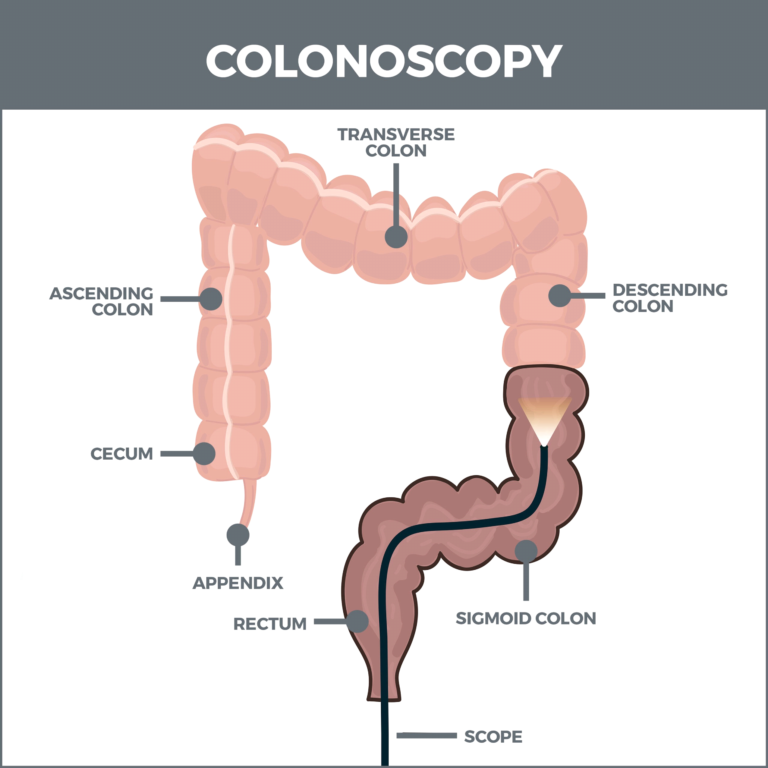
A colonoscopy is an exam used to look for changes such as swallon, irritated tissues or cancer in the large intestine. During a colonoscopy, a long, flexible tube is inserted into the rectum. A tiny video camera at the tip of the tube allows the doctor view the inside of the entire colon.
Why should we need a colonoscopy?.
A colonoscopy may be therapeutic or preventive. You are advised to have colonoscopy for routine cancer screening if you are at a statistically higher risk of developing colorectal cancer. Anyone can have colorectal cancer at anytime without warning or symptoms, screening is the best way to stay ahead of it. While screening your gastroenterologist may also remove suspicious tissues for testing.
Screening
Most people will have their first colonoscopy for routine cancer screening. Statistically, your risk of developing colorectal cancer goes up as you age, which is why the American Cancer Society recommends regular screening at least by the age of 45. You may not have any reason to suspect you’re at risk of colorectal cancer, but when your statistical risk goes up, it’s best to check anyway. Colorectal cancer often doesn’t cause any symptoms until it’s too advanced to treat effectively.
You may be due for a colonoscopy for cancer screening if you:
- Are older than 45 and haven’t had one.
- Haven’t had one for 10 years.
- Had tissue removed during your last colonoscopy.
- Have a family history of colorectal cancer.
- Have an inherited disease that raises your risk, such as familial adenomatous polyposis (FAP) or Lynch syndrome.
- Have inflammatory bowel disease.
Symptoms of colonoscopy:
- Unexplained rectal bleeding or discharge.
- Unexplained changes in your bowel habits, such as diarrhea, constipation or incontinence.
- Unexplained persistent abdominal pain.
- Unexplained weight loss or lack of weight gain in children.
Colonoscopy risks:
While a colonoscopy in itself is relatively safe, there are several factors that could contribute to problems during the procedure. If a doctor removes a polyp during the test, for example, your chances of complications may increase slightly.
While very rare, deaths have been reported following colonoscopies, primarily in people who had intestinal perforations occur during the test.
Risks associated with colonoscopy include:
- Bleeding
- Bad reaction after anesthesia
- Infection
- Colonoscopy prep risks
- Belly pain
- Discomfort
Problems after colonoscopy:
Postprocedure problems may include:
- feeling bloated or gassy if air is introduced into your colon during the procedure and it starts to leave your system
- a slight amount of blood coming from your rectum or in your first bowel movement
- temporary light cramping or abdominal pain
- nausea as a result of the anesthesia
- rectal irritation from the bowel prep or the procedure
How to Prepare for a Colonoscopy?
- Step 1: Plan Your Prep
- Step 2: Tweak Your Diet
- Step 3: The Fast
- Step 4: The Purge
Step 1: Plan your prep
Clear your schedule for the evening before and the day of your colonoscopy, and make plans for someone to go with you the day of the colonoscopy.
Shop for some key supplies several days ahead, too. Your list may include:
- A prescription or over-the-counter laxative specified by your doctor
- Low-fiber food
- Sports drinks, juices, and broths
- Moist wipes
- Diaper cream
Step 2: Tweak your diet
You can help the cleansing process by eating light 3 or 4 days before the procedure. Doctors recommend low-fiber foods that are easy to digest and leave your system quickly.
You can have:
- Eggs
- Chicken or fish
- White bread, rice
- Pasta
- Fruit without skin or seed
Do not have:
- Seeds, nuts, or popcorn
- Fatty foods
- Tough meat
- Whole grains
- Raw vegetables
- Fruit with seeds or peel
- Corn, broccoli, cabbage, beans, or peas
Step 3: The Fast
The day before your procedure you can’t eat anything solid. You should only consume clear (see-through) liquids. It is important to stay hydrated by drinking lots of clear liquids, such as sports drinks, clear juice like apple and white grape, and clear broth. Soda is OK, and so are coffee and tea, but without cream. You can have gelatin and ice pops, but stay away from anything colored red, blue, or purple. The dyes can discolor the lining of the colon and make it harder for the doctor to see. Also avoid alcohol and drinks you can’t see through, like milk or orange juice.
Step 4: The Purge
The night before your colonoscopy you’ll take strong laxatives to clear your digestive tract. The method recommended for most people is called split dosing. You’ll drink a half-gallon of liquid laxative in the evening. Then you’ll get up about 6 hours before your appointment to drink another half-gallon.
You probably won’t enjoy the taste of the solution, but there are tricks to help get it down:
- Mix it with something flavored, like a sports drink or powdered drink mix.
- Keep it well chilled.
- Drink it through a straw placed far back on your tongue.
- Follow it with a sip of something good tasting.
- Suck on a lemon slice or piece of hard candy after drinking.
Once the laxative starts working, you’ll have frequent, forceful diarrhea. You may have cramps and bloating. If you have hemorrhoids, they may become irritated. You may also feel nauseated and even vomit.
Try these tips to make yourself as comfortable as possible:
- Stay in the bathroom — bring something to entertain yourself, like a book, television, or laptop.
- Apply diaper cream before the diarrhea starts.
- Use moist or medicated wipes to clean yourself.